Diffuse Abdominal Pain
"Mr. Halpert, what seems to be the problem today?” you ask as you scroll through his unremarkable medical history on your tablet. On paper he looks completely healthy. His heart rate is slightly elevated -- probably due to the pain --but all of his other vital signs are within normal range. He looks pale and slightly diaphoretic.
His face is tight with pain as he says, "Please, call me Jim.” He groans and continues through a grimace, "Sorry about this. This is really embarrassing. I've been having pain for a few days. I thought it was just a bad burrito or something. I don't normally come to places like this, but the pain seems to be getting worse.”
Abdominal pain is the most common cause for hospital admission in the US. It represents a wide spectrum of conditions from food poisoning to appendicitis. Jim's pain could be caused by something as mild as emotional upset over his annoying coworkers, or it could be as serious as a perforation of the gut that needs immediate emergency surgery. You've got plans for a barbecue right after work, and in fact, your friends have already started without you. They've been texting you to get moving and join the fun. The last thing you want this evening is a prolonged session with a patient. You know from experience that an efficient assessment is the key to clocking out on time. What questions could you ask to get to the root of the problem as quickly as possible?
The Root Of The Problem
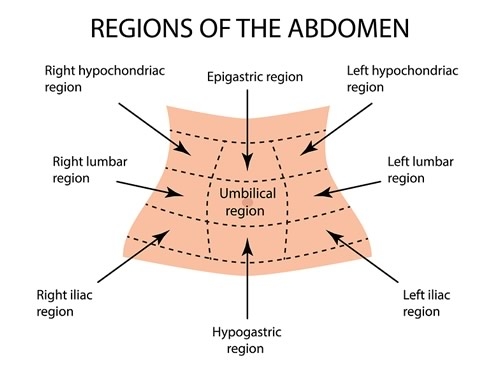
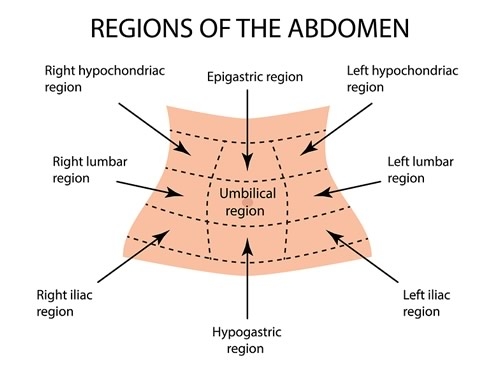
I'll bet you're thinking of one question, in particular, ...one that makes you want your pathophysiology textbook. There's a picture in there that will help. You know the one...it's an image of a torso with a tic-tac-toe board drawn over it. Each quadrant has a list of possible problems related to...LOCATION!
Before you click on either of the references below for help solving this problem, take out a sheet of paper and see how many possible problems you can list (no peeking!)
A Thorough Pain Assessment
You feel Jim's forehead with the back of your hand, even though you've already taken his temperature. It's cool to the touch. "Where, exactly is the pain?”
Jim says, "In the middle, right here" and clutches his abdomen right above the umbilicus.
"It's up above your belly button?” You ask and he nods in affirmation. "Not down below.” You point to your own belly, circling the area below your umbilicus. He shakes his head back and forth. "Is it worse on either side?” You point to your right and left abdomen as you ask the question.
"Maybe just a little bit worse on the left, but I'm not really sure.” He lightly pats his stomach with his left hand right below his breast bone.
"On a scale of 0-10, with 10 being the worst pain you've ever had and 0 being no pain, what is your pain right now?”
Jim thinks for a moment and then says, "I broke my leg playing football in college, and it's nowhere near that bad. I guess it's around a five or a six?”
You feel a sense of relief that his pain isn't severe. You know that in mildly ill patients watchful waiting and diagnostic evaluation is often the best approach.
The Options
Here's a list of the more common reasons for diffuse abdominal pain (we're going to look at these first...though it is possible he could have typhoid fever, it's not very likely!)
-
Pancreatitis
-
Gall stones/Cholelithiasis
-
Gastroenteritis
-
Peritonitis
-
Gastritis
-
Peptic ulcer
What else do you need to know to narrow this down? Make a list of questions you'd like to ask Jim.
History Lesson
I'm hoping your list of questions looks something like this:
-
Pain: location (check!), severity (check!), radiation, movement, onset, duration, severity, quality, exacerbating and remitting factors.
-
Associated symptoms: fever, anorexia, vomiting, syncope, GI blood loss
-
Medications: NSAIDs, prednisone, anticoagulants
-
Psychosocial: Drug and alcohol use, prolonged stress
Jim asks, "What do you think is wrong with me? Could it be food poisoning?”
You respond, "That depends. Let me ask you a few questions to help me narrow down what it might be. First off, does the pain radiate at all?” Jim shakes his head back and forth. You continue, "Does it get worse with movement?”
Jim replies, "No, not at all. It comes and goes. There's nothing that really seems to make it worse... or better for that matter.”
You continue, "You said it started a few days ago? Is the onset of the pain linked to anything you were doing?”
Jim pauses to think for a moment, "I can't think of anything. I guess I mentioned I went out for Mexican food with some friends.”
You ask, "Did any of them get sick?” He shakes his head no. "Have you had any vomiting or diarrhea?”
"Yeah, a little diarrhea, but I haven't thrown up. I do feel a little sick to my stomach occasionally. I guess that means it's not food poisoning, huh...It's weird...I haven't wanted to eat at all. Every time I try to eat something, I feel full right away. I guess that's why I thought it was something I ate.”
You add, "Food poisoning usually comes on pretty quickly with some fairly unpleasant side effects, but we're not ruling anything out yet. Have you noticed any blood in your stool?”
Jim turns slightly red and says, "No, I mean, not that I've noticed.”
You ask, "Have you ever had anything like this happen before?” He shakes his head back and forth. You continue, "Try to describe the pain for me. What is it like?”
Jim replies, "It's horrible!...but I don't think that's what you mean...”
You give a sympathetic smile and say, "Is there any cramping? Is the pain sharp, or more like a dull ache, does it come in waves?”
Jim responds, "No, there's no cramping, no waves. My stomach is tender though if I press on it, it hurts. I guess the best way to describe it is kind of a gnawing or burning pain, if that makes any sense? And it comes and goes...and I have lots of indigestion like I said...no appetite and feeling nauseated. I'm just so tired…”
You look up from typing in Jim's symptoms to ask, "Tired of being in pain?”
Jim answers, "Yes that, but also just tired all over. All I want to do is sleep, but I can't because of my stomach.”
You nod and pick up the tablet, "I hear you, it's hard to be in pain for a few days. It's good that you came in. I'm going to have the physician come in here in a sec, and she's going to do a more thorough exam. I just have one final question.”
What Is It?
There's one question that will really seal the deal here. What's one thing from this patient's history that might give you a big clue to what is causing his abdominal pain and get you out of work on time?
Stay tuned for the exciting conclusion! I'll post the final puzzle piece of Jim's history, and give you some diagnostic clues as well. Feel free to ask questions and make comments below.

 I think the next question to ask is if the pain is typically worse a few hours after a meal. After the stomach is emptied.
I think the next question to ask is if the pain is typically worse a few hours after a meal. After the stomach is emptied.
SafetyNurse1968, BSN, MSN, PhD
60 Articles; 529 Posts
Thanks for your patience with this, we are trying out a new format, next time I’ll post a lot more quickly so you won’t have to wait so long. In a couple days I’ll post the actual diagnosis!