- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education

beekindRN, ASN, RN
47 Posts
I participated in a code yesterday that was textbook. Everything went as expected, but the overall prognosis for the patient was extremely poor. This was her fourth (and seemingly endless) code in just a couple hours.
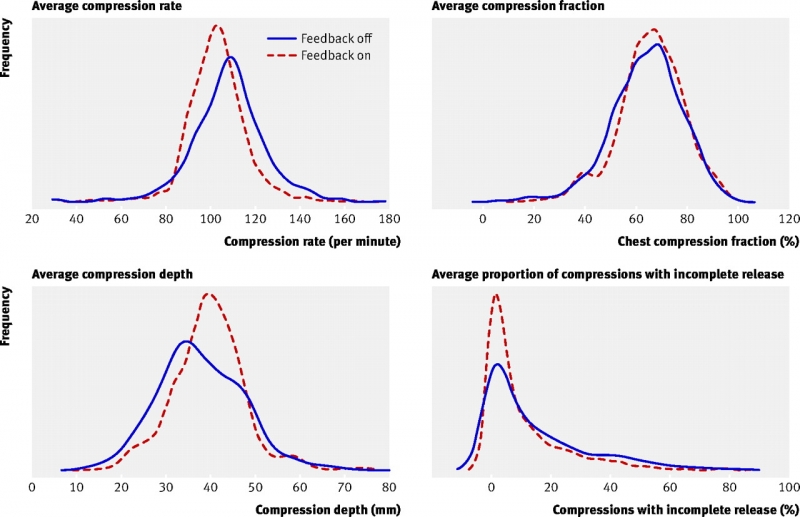
My question is we had two nurses who were absolutely jackhammering their compressions. I thought it quietly but didn't say anything, as I'm a new nurse and didn't want to argue during a code and potentially compromise quality care. I also accepted that our efforts were most likely futile anyways. However, an aide who is in nursing school later pulled me aside and noted that these compressions seemed incorrect. She provided slow, deep compressions and even started she was humming "Stayin' Alive" to maintain a proper beat. She was berated briefly during the code by a nurse for performing "tired" compressions due to her "slow" rate, but I thought she allowed for complete chest recoil and maintained an even, appropriate rhythm.
Next time, how do I address incorrect compressions professionally and appropriately?