Ms. Grant (not her real name), a 68-year-old woman, recent cardiac bypass
Postoperative for elective cardiac bypass with significant complications: ventilator acquired pneumonia, right-hemispheric stroke, clinically significant GI bleeding, acute tubular necrosis requiring hemodialysis
Stated on the morning of the event: "I feel good for the first time in a long time."
Morning of a planned transfer to step-down patient was observed coughing and moving head and extremities in an uncontrolled manner. BP 220/95 mmHg.
No history of seizure or seizure medications
Blood was drawn, the patient was taken for a CT to rule out a stroke or cerebral hemorrhage
Serum glucose came back 0 during transport to CT lab
The patient died after being in a coma on life support for 7 weeks.
What happened here? A woman well on her way to recovery from a difficult postoperative course was about to be transferred from the ICU to a step-down unit. What caused the seizures? Keep reading to find out (Link to full article is at the end of this blog post)1.
Medical Error
The Institute of Medicine published a report in 2000 called "To Err is Human"2. This report is based on thousands of chart reviews from various hospitals in the late 80"s and 90's. Americans were shocked to find out that medical error kills the same number of people as if a jumbo jet full of passengers crashed every week, with no survivors - approximately 44,000-98,000 deaths per year. These numbers are likely a gross underestimate, with the true number being closer to 400,000 deaths per year.3Recent research suggests medical error is the third leading cause of death in the US. In a report from the British Journal of Medicine in 2016, the authors analyze how medical error fits in with the leading causes of death (heart disease and cancer are still 1 & 2) with lower respiratory disease being 3rd and accident 4th.4
I think it's safe to say that almost no one in healthcare wants to make an error. Despite our best efforts, we continue to harm patients (I talk about this in another blog post. This list shows the most common medical errors.
Medical Errors
-
Adverse Drug Events6
-
Catheter-Associated Urinary Tract Infection
-
Central Line-Associated Blood Stream Infection
-
Injury from falls and immobility
-
Obstetrics
-
Pressure ulcers
-
Surgical site infections
-
Venous thrombosis
-
Ventilator-Associated Pneumonia
The National Patient Safety Foundation has a Vision Statement: Creating a world where patients and those who care for them are free from harm.5 We can also most likely agree that our goal is for patients to be free of harm - specifically preventable accidental harm. We cannot eradicate human error, but we can build safeguards where we know error is likely, thereby decreasing the impact of errors and potential for harm.
Timeline
Back to the case study. Have you come up with some ideas for what happened to Ms. Grant? Take a look at this time line from the actual incident to give you some additional information.
|
Time
|
Event
|
|
0430
|
Nurse draws blood for routine morning laboratory tests: serum glucose level is 6.72 mmol/L (121 mg/dL)
|
|
0600
|
Medical student visits patient before team rounds. Patient is stable
|
|
0610
|
Cardiothoracic ICU team visits; no new issues are noted. Patient is showing much improvement; team has every expectation that she will make a complete recovery
|
|
0620
|
Patient drinks small amount of orange juice; note in chart indicates patient is stable
|
|
0635
|
Nurses uses a straight urinary catheter to drain a patient's bladder per standing order. Patient appears well by tired; expresses a desire to nap.
|
|
0645
|
The alarm goes off, alerting nurse to occlusion of the patient arterial line; nurse flushed line with 2 mL of heparin lock flush.
|
|
0735
|
Day nurse receives shift change report from night nurse and assumes care of the patient.
|
|
0745
|
Night nurse completes shift. Patient is reported to be sleeping soundly
|
|
0815
|
Day nurse discovers a patient having seizure activity. Labetalol is given by day nurse for systolic BP >200 mm Hg. Patient physician is called.
|
|
0820
|
1 mg lorazepam given IV by the nurse for an apparent seizure
|
|
0835
|
Neurology is called for an abrupt change in LOC
|
|
0842
|
Emergent CT whos no evidence of intracranial hemorrhage, mass or mass effect. Lab notifies ICU that serum glucose is undetectable. 1 ampule 50% dextrose in water given IV
|
|
0855
|
1 mg lorazepam IV
|
|
0905
|
1 mg midazolam given IV push, patient intubated
|
|
|
|
Where in this time like could an error have occurred that cause Ms. Grant's death? I want to emphasize that she didn't die from any of her multiple post-operative complications. Ms. Grant died as a direct result of an unintended, preventable medical error that occurred between 0430 and 0815.
Here is the rest of the timeline, and the piece of information that will most likely lead you to the most obvious cause of her seizure.
|
0915
|
Day nurse discovers bottle of regular human insulin on medication cart immediately outside patient room
|
|
0920
|
1 mg midazolam IV push
|
|
0945
|
10 mg chlorpromazine, 6 mg morphine, 2 mg midazolam IV push
|
|
0950
|
1 ampule 50% dextrose in water given
|
|
1005
|
Glucose level of 1.3 mmol/dL (24 mg/dL) reported from lab
|
|
1015
|
1 ampule 50% dextrose in water given
|
|
1100
|
2 ampules 50% dextrose in water given
|
|
1245
|
5 mg labetalol given IV push for systolic BP of 195 mmHg
|
|
1315
|
1 ampule 50% dextrose in water given for serum glucose of 3.1 mmol/L (55 mg/dL)
|
|
Remainder
|
Blood glucose level difficult to maintain, patient comatose
|
After a thorough investigation of this sentinel event, it was discovered that at 0645, the nurse flushed the patient arterial line with insulin instead of heparin. Due to the presence of insulin on the medication cart, there is no way to determine if this was the first time this had happened.
Nursing Role
I'm teaching the fundamentals of nursing right now to brand new BSN nursing students. What follows is a description of what we teach them. The nursing role is to administer medication as prescribed while preventing error and patient harm.
What goes into "administering medication as prescribed"? In addition to being aware of federal, state, and institutional regulations, nurses also need to know the nurse practice act and their scope of practice.
Nurse Knowledge Of Medications:
-
Generic- given by the original manufacturer which becomes the drugs official name, vs. Trade- name under which the drug is marketed.
-
Look-alike/sound-alike drugs- list produced by the Institute for Safe Medication Practices and the Joint Commission.
-
Classification- indicates the effect of the drug on the body/site of action.
-
Medication Form- the form the medication comes in such as tablet, elixir, powder inhalation, often affects absorption and metabolism
-
Pharmacokinetics describes how a medication enters the body, reach and active state for action, metabolized, and excreted when their effects have been obtained
-
Therapeutic Effect- the expected, desired effect of taking a medication vs. Side effect- expected, unavoidable effects, at therapeutic doses. Adverse effect-undesirable/unpredictable side effects, often severe, Toxic effect- may be a result of prolonged exposure to drug or excessively high dosage, accumulation in the blood, may be lethal in their results
-
Idiosyncratic reactions- unpredictable over or under reaction of a patient to a medication I.e. Benadryl making a child climb the walls when it should really make them sleepy.
-
Allergic reaction- an immune response is elicited, release of antibodies by the body -Anaphylactic- life-threatening, reaction constriction of bronchiolar muscles, edema of the pharynx/larynx, severe wheezing, ShOB
-
Timing: onset, peak, trough, duration, half-life,
-
Route: Parenteral, SQ, I'm, IV, Non-parenteral, Oral, Sublingual- under the tongue, Buccal-mucous membranes of the cheek, Topical, Inhalation, Intraocular
-
Measurement: Metric- mL, mg, g, L, Household- drop, cup, tbsp., tsp. , oz.
The Five Rights
In addition, since 1893, we have been taught the 5 rights as the number one process for safe medication administration. The five rights were first seen in The Nursing Sister: A Manual for Candidates and Novices of Hospital Communities.7 Nursing sisters taught five rights to prevent error: right patient, medication, dosage, route and time. Since then, there have been an increasing number of rights: client education, documentation, client right to refuse, assessment, and evaluation of the client after the medication is administered.8The number of rights increases, but error rates do not change. I have tried to find research to support use of the 5 rights - there isn't much out there - no randomized clinical trials showing that using the 5 (or 6, 7, 8, 9) rights improves patient safety when compared to some other method of safe medication administration.
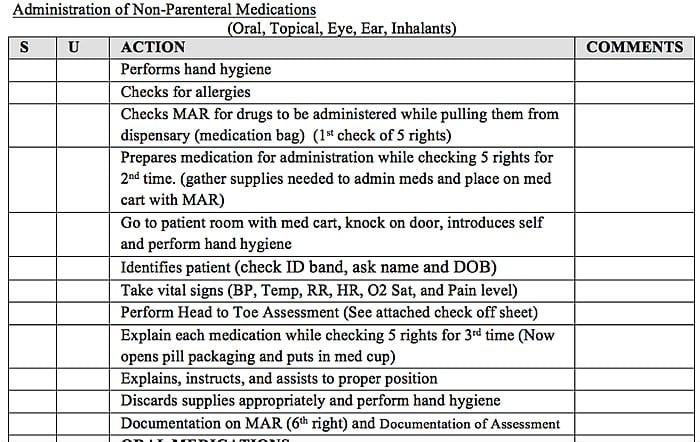
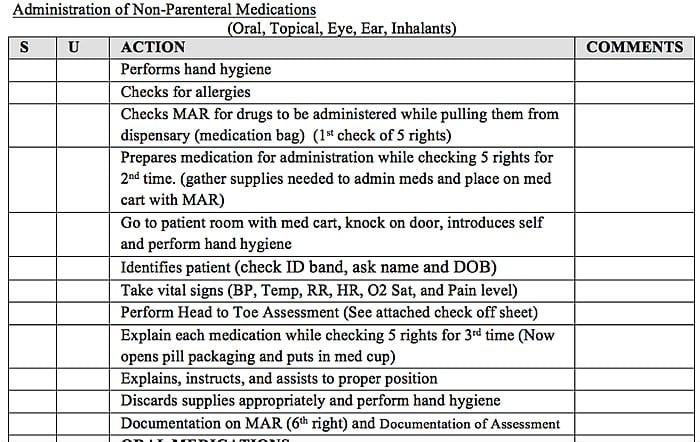
Below you will see safety guidelines from a fundamentals of nursing clinical packet. It's what we are teaching new nursing students to do to prevent medical error.
Safety
-
Maintains medical asepsis, sterile technique and standard precautions
-
Maintains proper body alignment and personal safety
-
Demonstrates appropriate use of equipment provided
-
Provides nursing care that maintains the emotional and physical safety of patients
-
and other members of the healthcare team
-
Demonstrates knowledge and identification of national patient safety goals
-
Communicates observations or concerns related to hazards and errors to patient,
-
Families and the health care team, and faculty
-
Organize multiple responsibilities and provide care in a timely manner while using
-
clinical reasoning skills to prioritize care
-
Safe
-
Accurate (each time)
-
Affect (each time)
-
With occasional or with supporting cues
And here is a clinical check-off sheet for a return demonstration for safe medication administration
Blame The Nurse
It's obvious that the nurse who gave the patient insulin instead of heparin made a mistake. That nurse gave the wrong drug. That nurse didn't follow the five rights. If we stop with these statements, is it possible this error could happen again to another patient? The answer is YES. We have to go deeper if we want to prevent error. "The single greatest impediment to error prevention...is that we punish people for making mistakes" Dr. Lucian Leape9
Getting To The Root Of The Matter
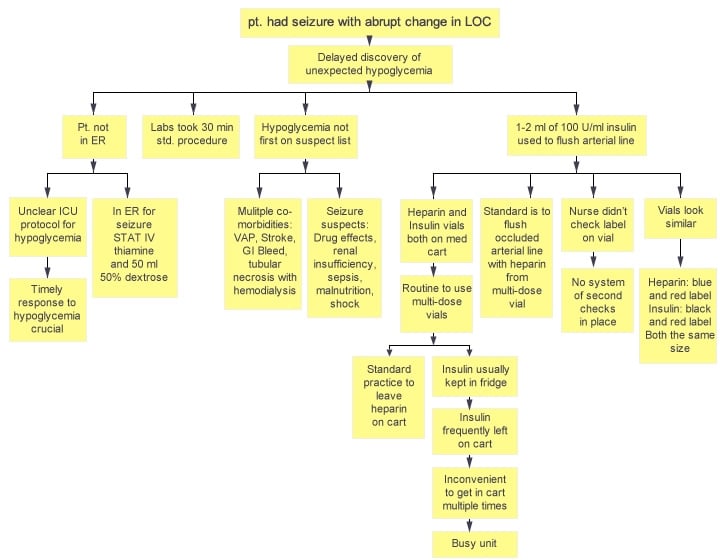
Doing a root cause analysis is required by the Joint Commission for sentinel events (I wrote about RCA in another blog. Below is the causal tree from the RCA for Ms. Grants death.
Solutions
The causal tree shows that multiple factors contributed to the patient receiving the wrong drug. The committee that investigated the death came up with the following solutions:
-
Insulin was added to the automated dispensing device
-
Staff were educated to keep medications secured and not on drug cart
-
Nurses were reminded to keep med carts locked
-
Use of multi-dose vials of insulin and heparin prohibited
-
Use of saline flushes to restore patency of arterial lines required instead of heparin
-
Interdisciplinary team to examine how to expedite delivery of medications to patients
At the end of every Root Cause Analysis (I have lead many as a former Patient Safety Officer) we always ask, "If these interventions had been in place at the time of the event, could the error have occurred?" If the answer is "yes" then we get back to work. What do you think? Are there any other ideas you have for preventing this type of error? What experiences have you had with medical error?
Second Victims
A "second victim" is a healthcare worker who has been involved in a medical error. Second victims often experience emotional trauma, stress, financial strain, loss of job and loss of peer respect after being involved in an error. Unfortunately, I've been there (yet another blog)
If you or someone you know has been involved in a medical error, please send them to one of these sites to get support and help:
ProPublica Patient Safety Action Network Community: Patient Safety Action Network Community Public Group | facebook
Medically Induced Trauma Support System: Home - MITSS
REFERENCES
Bates, D. W. (2002). Unexpected hypoglycemia in a cricitally ill patient. Annals of Internal Medicine, 137(2), 110-116. Retrieved from: Unexpected Hypoglycemia in a Critically Ill Patient | Annals of Internal Medicine | American College of Physicians
Kohn, L., Corrigan, J., & Donaldson, M. (2000). (Editors). To err is human: Building a safer health system.Washington DC: National Academy Press.
Classen, D., Resar, R., Griffin, F. (2011). Global "trigger tool" shows that adverse events in hospitals may be ten times greater than previously measured. Health Affairs, 30, 581-9. doi: 10.1377/hlthaff.2011.0190.
Makary, M. & Daniel, M. (2016). Medical error - the third leading cause of death in the US. British Medical Journal, 353, 1-5. doi: 10.1136/bmj.i2139
Institute for Healthcare Improvement
Wachter, R. M. (2012). Understanding patient safety. 2nd ED. China: McGraw Hill.
Wall, B. (2001). Definite lines of influence: Catholic sisters and nurse training schools. Nursing Research, 50(5), 314-321.
Potter, P. A., Perry, A. G., Stockert, P., & Hall, A. (2013). Fundamentals of nursing (8th ED.). Philadelphia, PA: Elsevier.
Leape, L., Epstein, A. M., & Hamel, M. B. (2002). A series on patient safety. Journal of the American Medical Association, 288(4), 501-508.
Patient Safety Action Network Community Public Group | facebook
Home - MITSS

Life's Too Short, ADN, LPN
1 Post
Long time reader, first time poster.
This one struck a chord with me as I almost made this exact mistake. Order for 5000 units/1ml heparin subQ q8hr. Our heparin is dispensed in individual vials. Though individual patient meds are pulled and stored in individual drawers on our wow's. It is (was) not uncommon to find a vial of humalog or humalin sitting on top of the wow as these are 'multi draw' vials. I had scanned this patient, scanned the heparin and set it on the wow. You can see where this is going. I was talking to the patient and answering questions from her grown daughter as I drew up 1 ml of lispro into a TB syringe!
Fortunately I routinely stop just prior to giving meds to the patient to recheck everything. When I looked at the heparin vial and noticed the orange cap still intact, my stomach dropped, as I realized what I had done.
Somehow I remained composed with the patient, walked over to the sharps and dropped that 100 units of lispro in and started over. As I left the room, visibly shaking at what could have happened, I count my blessings that my Fundamentals teacher drilled us with the 5 rights over and over and over again. Thank you Ms Jackson!
I shared the incident with my manager, wrote up a 'near miss' incident report, and continue to share this story with other nurses on my unit , especially new nurses. You will never see a vial of insulin (or anything!) sitting on my wow unless I am preparing that dose. When I see a vial on someone else's wow, I will secure it. Overstepping? Maybe. But we wouldn't leave an oxy laying around, and a vial of insulin could do a lot more damage.
Slow down, pay attention and check, recheck, and check again.