- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education

deepurple
139 Posts
Hi everyone...i want to ask for help about the care of chest tube. I list the responsibilities of nurses for chest tube care. From your experiences, is there any info to add in the list below from all of you. TQVM, You're most welcome.
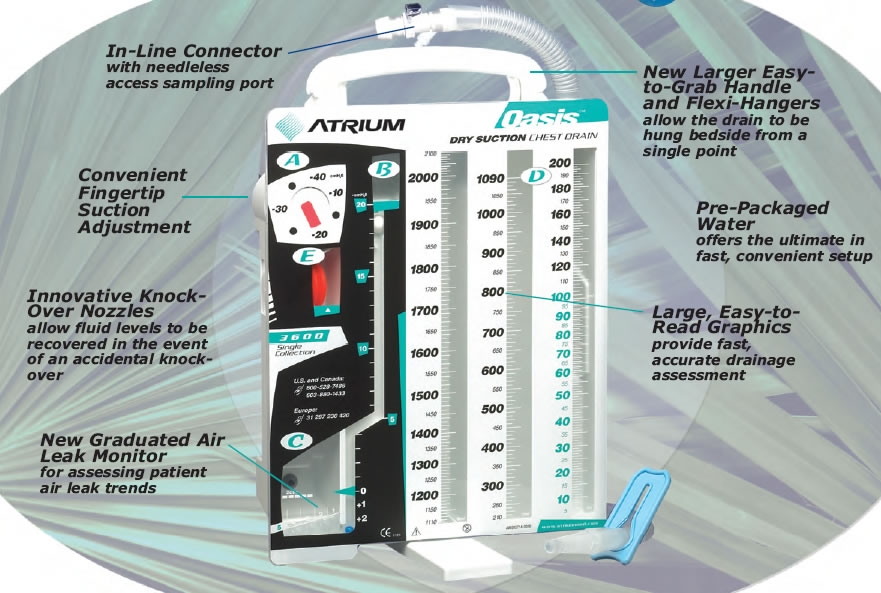
1.Check dressing at the site of chest tube insertion
-Ensure the dressing or plaster is intact to avoid the chest tube is slip out.
2.Do dressing at the chest tube insertion site to avoid potential infection.
3.Check the patency of the chest tube
- Do milking or stripping along the chest tube to avoid blockage or obstruction of the drainage.
4. Observe the type of drainage and amount of drainage.
5. Check is there any bubble in the chest tube to to know whether there is pneumothorax
6. Change the drainage bottle when 2/3 full of drainage.
- if chylothorax - need to change the drainage bottle everyday to observe the progress of the drainage.
7. Clamp the chest tube when to move the patient or when to walk to avoid the back flow of the drainage into the lungs or cardial.