- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education

Esme12, ASN, BSN, RN
20,908 Posts
There are requirements of EMTALA that are required to apply to ALL patients regardless of their ability to pay or insurance status
I worked emergency Departments before these anti-dumping laws and there are very good reasons why these laws had to be enacted and enforced.Now here is where EMTALA can be "adjusted" and I have heard of some facilities out west that are "attempting" this interpretation differently.
In EMTALA patients are required to have a MSE (Medical Screening Exam) This is NOT a triage assessment by the nurse.
These facilities have developed their own sort of "urgent care" where a mid-level provider is involved to the triage process to determine IF a medical emergency condition exists......Now just because a physician is not in violation of EMTALA for turning away a PE for muscle strain doesn't mean they can't be sued...however again this patient was NOT turned away at triage and sent on their way due to lack of payment/insurance and told.....and if they are it is the mid-level provider or MD that makes that determination and NOT the triage nurse.Now EMTALA does not require a hospital to self report so you can't tell on yourself and get fined so if no one complains that you get off scott free....until you are caught and loose you medicare/medicaid CMS approval and stop receiving medicare payment. Which is highly unlikely a hospital will risk losing reimbursement especially when they are being reimbursed effectively
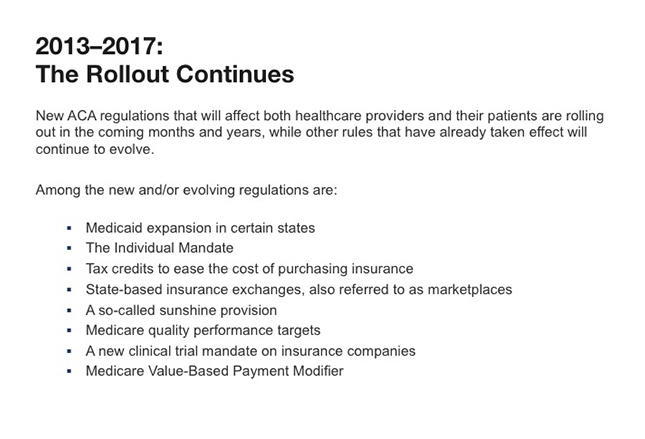
If you with to read more about EMTALA....COBRA Laws and EMTALA through medscape.....it requires registration but it is free and an excellent source of information.So I do not see how the ACA affect emergency department visits unless it will be in the form of payment to the facilities that don't include the federal government because some of the uninsured will now have to pay hefty premiums to insurances companies who the pay the provider. I see the big money conglomerates just getting more money to line their pocket with little actual regard to whether or not people actually get sufficient care.
I live in a state that already has this as law and a very litigious state....it has done nothing to relieve the burdens of local emergency departments and lengthened the time it takes to see any PCP. I feel the quality of care has diminished when it is quantity that pays. You are allotted 10 mins for a visit. period...$40.00 co-pay and they bill your insurance co. $380.00 I have actually offered to pay for 2 office visits so I can feel like they hear ME and NOT the clock ticking saying time out. Concierge medicine is now in fashion....for a steep monthly fee....now that has improved healthcare for those who need it most.