- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education


Duty Calls
In the wee hours of a pitch-black Pacific northwest morning, I’m jolted out of a dream by the grating sound of my alarm. The air is still and crisp and this bed, full of toasty dog and human bodies, isn’t exactly an incentive to move my tired bones. I’m exhausted to my core, a not-too-unfamiliar feeling held by bedside nurses, compounded by an epidemic that overnight has transformed our hospitals, our profession, and our world. But duty calls, night nurses are weary, and people are dying.
Download allnurses Magazine
Breathing Clean Air - A Precious Commodity
With my precious family safe and sound, the fear of bringing home this silent visitor not only weighs heavily on me, but especially for parents and those with their own aging parents to protect. Coffee in hand, I slip out the door and slide on my clogs waiting dutifully on the back porch, a common practice when the enemy clings to your feet. Just a few months ago no one had heard of it, this deadly invader - Coronavirus, Covid-19, SARS Cov-2 to name a few of her aliases. Now Corona is on everyone’s hearts and minds (and hands and metal surfaces for that matter). She’s finally gotten the wake-up call essential to thwart a pandemic this vicious in spite of feet-dragging leadership from the current administration. Rather than repelling from crisis, we nurses and other medically trained citizens, head directly towards it like firefighters to a burning building. Things previously taken for granted like thoughtlessly breathing the air around us, or our job security; are now both precious commodities.
Nurses Swarm the Hospital
Like a buzzing hive, nurses swarm the hospital decked out in full personal protective equipment, or PPE as we say: blue-gloved and wrestling with negative pressure helmets like awkward astronauts navigating life without gravity. In the first and last hours of the workday, a hospital hosts double the staff as night and day shift nurses hand off stories and requisite details of the past twelve hours, information that can’t be gleaned from perusing charts alone. One of the beauties of nursing is leaving your grueling shift behind you and passing it on to the next highly-capable nurse. It’s her turn now, and with a rested mind she eagerly gets a breakdown of what’s in store. Today I’m charged with three step-down patients on telemetry- in other words, they aren’t sick enough to require one-to-one observation, but they do require being placed on a heart monitor and haven’t be cleared to leave ICU.
Lives at Stake
New policies seem to surface by the hour, the newest one being mandatory use of OR scrubs which add to the look of an insect colony. The endless stream of indiscernible teal-green nurses stride up and down ICU hallways 24/7. In his renowned book, The Superorganism: The Beauty, Elegance and Strangeness of Insect Societies, Harvard biologist Edward O. Wilson described the extraordinary lives of social insects and how they cease to be individuals but rather function as a single organism. These superorganisms are formed by “altruistic cooperation, complex communication, and division of labor” much like these teams of front-line healthcare workers at the heart of this epidemic. Every member of the colony has a job to do and their altruism is what makes them so successful. The beauty and grace with which they execute critical health care so adeptly is quite moving, knowing that both patients' and nurses' lives are at stake.
The newly coined ‘COVID row’ in ICU is an impossibly long hall of glass doors and shiny equipment carts, bays occupied with unconscious prone bodies, like sunbathers leisurely napping on a noisy crowded beach. Nurses peek through their isolation suits secluded further behind glass. They write their requests with dry erase markers, while non-isolation nurses act as runners for supplies, medications, and delivery of crucial labs for testing.
By mid-morning I’m lending a set of hands to the rounding team flipping patients every eight hours in a last-ditch attempt to increase lung expansion and in turn, oxygen levels. That being said, once they have reached this point, the general consensus is that they will almost never pull through.
Daily Updates
We learn more and more about this nasty intruder on a daily basis, like how there seems to be no rhyme or reason to who and why it hits hardest. The virus now appears to affect not just the frail and elderly but young people too, with very few medical problems. Unusual new tidbits of information creep in daily, like COVID’s connection to hyper-coagulation which can lead to devastating, widespread blood clots and even more anomalous, a loss of taste and smell.
No Time to Pee
It’s noon and I haven’t had a single break, eaten, or peed since I walked on to the unit this morning. Nurses will admit, it’s easy for us to neglect our own basic human necessities when a patient’s unmet needs mean someone is suffering. I ask another nurse across the hall from me to keep an eye on my call lights while I take a much-needed lunch and bathroom break- just enough time to recharge and get back on the floor.
Ventilators
I’ve been recruited to pull and sign off on sedation medications designed to optimize comfort for these patients who are intentionally paralyzed in an effort to minimize every ounce of oxygen use while on ventilators. Once patients are dependent on these vents, more often than not it becomes the point of no return, critical-care trained nurses strait-forwardly identifying who will make it and who won’t based on impressive levels of experience and intuition. A maze of tubing and wires surround monitors working around the clock to tell us what we need to know to keep patients alive.
Lack of Testing
The elephant in the room is that few of us nurses are being tested proactively regardless of our being at the highest risk of exposure and in turn exposing others. Without overt symptoms, the protocol doesn’t call for testing, and a positive test means loss of income for us too. The reality is that COVID-positive nurses means no one to take care of patients who just keep coming.
Emotions run high among staff with an influx of daily emails informing us of test results from now COVID-positive patients we’ve had contact with. Caring for so many patients on a daily basis, it’s often difficult to put a name with a face trying to remember precisely how careful you were in protecting yourself. Rationing face masks, reusing equipment, running out of disinfectant wipes is the new normal and we are all acutely aware of how we are putting ourselves, and in turn our families at risk.
Up Close and Personal with COVID
Being up close and personal to this virus is both humbling and frightening. Our nurturing personalities allow us to lean in to the discomfort, but the fear remains. We want to save lives and use our knowledge to ease suffering but at what cost? Results continue popping up positive faster than the hospital’s lab can process results, and the sickest patients are being put on comfort care, essentially ending any further treatment designed to cure them.
The pressure cooker finally began leaking steam, taking its toll with the onslaught of media reports, worried friends and family, and a hospital understandably not equipped for what COVID brought through its doors. Two shifts prior, I was in a patient's room every hour on the hour for an unrelated medical problem that got him admitted to our unit and had since tested positive for Corona.
The most obvious problem is that all of us, nurses, techs, doctors, respiratory therapists, speech pathologists, physical and occupational therapists, the environmental and food service workers — we’ve all been exposed to some degree. Isolation carts are under-stocked or offer only simple surgical masks, ineffective for airborne viruses which is what Corona becomes once aerosolized by breathing treatment nebulizers and CPAP machines for patients with sleep apnea. Previously non-isolated patients are getting orders to be ruled out for the virus after endless staff have been in and out of these rooms for days. We handle bodily fluids in all its forms on an hourly basis while the CDC and hospital administration are scrambling to keep us up-to-date with guidelines that change faster than they can be typed and distributed.
COVID-positive patients are moved to the outskirts of each unit in an attempt at isolation but the hospital initially had no choice but to mix them in with the general population. The environment in the hospital is nerve-racking aside from dealing with improper PPE equipment, reusing of old, contaminated masks, a lack of transparency with staff testing positive, and the higher-ups pushing back on offering critical pay. All we can do is dig deeper and scrub our hands a little harder, until the skin is raw, and faces are left grooved from N95 masks. We guard the cleanest PPE with our lives so no one helps themselves to this now-precious commodity. Fifteen minutes is all I have to empty my bladder, top off the tank, and get back on the floor.
Not Enough Critical Care Personnel
In truth, we simply don’t have enough critical care nurses or intensivists (critical care doctors) to manage these patients and because of it, ICU nurses delegate vital tasks right up to the limit of their scope of practice. A glut of extra nurses are out of work and on the unit-due to near-empty ORs and recovery rooms. Outpatient clinic nurses pace the halls as “helpers” and to ensure PPE is worn and removed properly, the only task they are permitted to do out of their home units. Other wings are eerily quiet without the usual influx of anxious family members and elective surgeries.
No Treatment or Cure - Supportive Measures Only
With no reliable treatment or cure while we wait for research to catch up, nurses cling to what we know-supplemental oxygen, IV fluids, adequate rest-the basics of supportive care. This isn’t the last pandemic we will see, but it is my first as a nurse. Deadly diseases are part of the human experience and mankind has coexisted with them since the beginning of time. But the effects of Corona will forever change the way we deliver nursing care and relate to other human beings as a society. We are social creatures and need human connection as much as we need oxygen to breathe. Intimacy is at the core of what we do.
Scared of Becoming a Statistic
Throughout the pandemic I’ve been depleted, enduring dog-tired days-on-end where I wasn’t sure how I’d muster the strength to come back for another twelve hours. I’ve felt both fortunate and guilty for the job security because people are dying, including hundreds of front-line workers-nurses just like me. I’ve felt humbled and honored to be the person at the bedside of dying patients unable to make contact with family due to restrictions on visitation. I’ve been scared to become just another statistic myself and felt the urge to hide in equipment closets so no one sees the nurse breakdown and cry too.
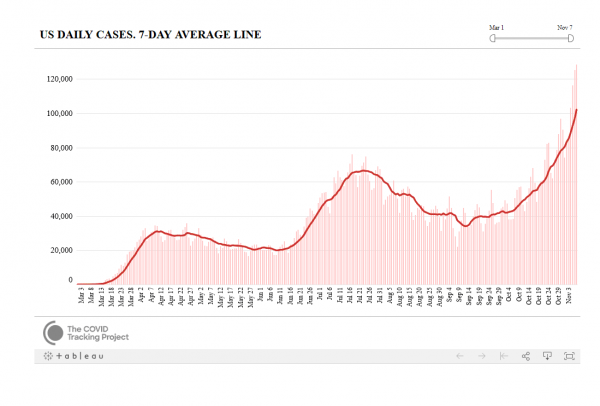
Nation's Failed Response
It's impossible not to recognize how our nation’s response has failed its citizens, how unprepared we were with a broken healthcare system so fixated on profit, and how blatant misinformation and ignorance allowed the virus to spread like wildfire, how Jeff Bazos and insurance company’s bottom lines are likened to war-time profiteering of yesteryear. Like landing on the moon and electing our first black president, we will forever split our memories into pre and post-Corona virus eras and nurses will forever remember the days when we didn't always wear masks.
Running the COVID Marathon
Every shift is like running a marathon and by four or five o’clock, you can just about see the finish line. That coffee you slammed down while your patient was off the floor for an MRI gives you enough kick to admit a new ED patient and catch up on charting before shift change. Experienced nurses know the importance of self-care habits like adequate sleep, turning off your brain at the end of the day, eating right, and all those things that allow our immune system to choreograph its exquisite dance of knowing what to kill and what to keep. But today I settle for simple moment of silence to reflect on what we just accomplished.
By a quarter ‘till seven, night shift begins trickling in and the mere sight of them inspires joy in us all. The handoffs commence like clockwork, as night nurses anxiously take control. Day shifters convene at cohort borders, stripping off contaminated scrubs and masks under the strict supervision of trained observers.
Tokens of Appreciation
I sit down for the first time in hours. Boxes of donated food, and thank you cards from the community have taken over break-room tables. There are hand-written notes from girl-scouts, homemade cookies, doughnuts, and gourmet meals from local restaurants-it’s overwhelming but always devoured. I wish I could find a way to tell them all that these meals are saving our lives too. Their words of encouragement and appreciation for taking care of precious loved ones make it all worthwhile.
“Thank you for your service!” a gal says to me in the Whole Foods parking lot. The comment catches me off guard having spent a grueling twelve hours on my feet, my brain running on fumes. I failed to notice the way scrubs cause a nurse to stand out more than ever. I’m just doing my job, I say to myself, just business as usual when you're a nurse. Not exactly a hero here. My father, a Vietnam era veteran, also always took the praise with ambivalence, feeling he was simply a cog in the corporate-American wheel. I’m not exactly used to having the entire world shining a spotlight on what I do every day, but admittedly, it’s incredibly comforting to have this sudden connection to complete strangers. I too have always been uncomfortable with being the center of attention but like I coach my father into doing, I smile gratefully and say, you’re so welcome.
A Nurse at Ground Zero WORD 8:12.docx
About Robin Queen
Robin Queen is a cardiology travel nurse turned health and travel writer/Certified Culinary Medicine Specialist. She currently lives all over the globe and can usually be found in tropical waters, surrounded by animals, or devouring the best food a region has to offer.
Share this post
Share on other sites