- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education

kathleenweels
2 Posts
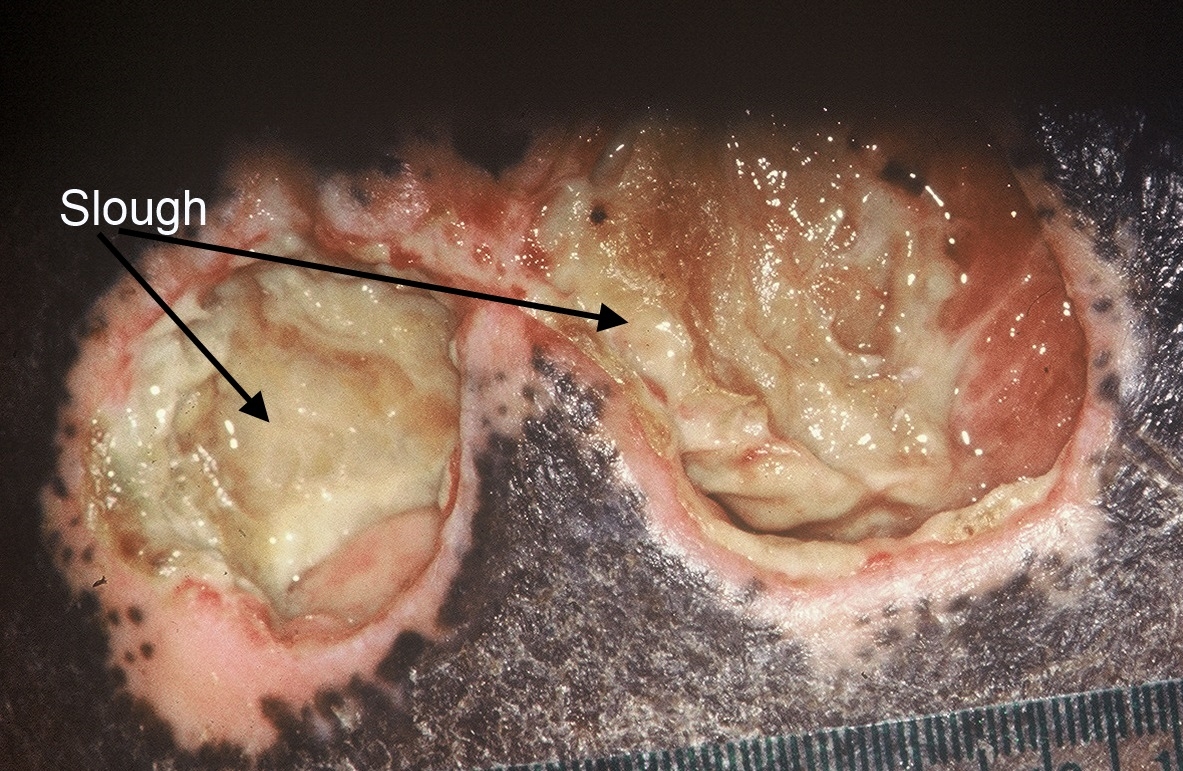
Hello! I'm a home healthcare nurse and I have my first patient with a wound vac - he had a left AKA and the wound badly dehisced. He has a complex history of vascular disease, anemia and diabetes. I am concerned that the wound bed today had a slough or yellow color to it when I changed the wound vac. Is there a typical color it should be? i know that pink/beefy red granulation tissue is the goal, but when should I be expecting to see this color? This is the second time i've changed his wound vac. any input would be appreciated, thanks!!!