-
allnurses (Editorial Team / Admin)
Nurses form the backbone of the healthcare system. The U.S. has approximately 5.2 million active nursing licenses. Occupational hazards and unhealthy lifestyle behaviors increase nurses' risk for cancers like breast, colorectal, and hematological malignancies. In addition, working night shifts is linked to circadian stress and cancer development. As cornerstones to patient care and healthcare delivery, these increased cancer risks underscore these nurses' need for support after a cancer diagnosis. Supporting nurses in returning to work after a cancer diagnosis can support their well-being and the viability of the workforce.
Although there is a growing interest in nurses' return-to-work experiences, important gaps still exist in our understanding of the factors that facilitate or impede this process. Most studies focus on general healthcare professionals without considering the unique positions and needs of nurses. There is also a lack of wide-ranging research on the long-term outcomes of return to work among nurses, including job retention, career satisfaction, and quality of life. These gaps must be addressed to develop evidence-based strategies and policies .
Challenges in Returning or Continuing to Work After Cancer
Cancer and its treatment affect not only the overall health of nurses but also affects many aspects of a nurse's work and quality of life. Lingering symptoms from treatment, such as fatigue, lymphedema, or pain, are experienced by many nurses, making it difficult for the physically demanding requirements of the job to be met, including prolonged standing and lifting. Cognitive challenges, commonly referred to as "chemo brain," and mental health concerns, including anxiety and depression, are known to influence their pace to return to their clinical positions.
Nurses often require work accommodations after a cancer diagnosis. These adjustments help them manage their health and fulfill their responsibilities. However, additional stress can be created by inconsistent workplace support, limited flexibility, and gaps in understanding from managers and colleagues. Nurses hold dual roles as healthcare providers and cancer survivors, which places them in a special position of vulnerability; thus, dealing with their physical and emotional needs is necessary during the transition.
Findings from Our Research
Our team has completed a scoping review to identify the knowledge gaps in nurses' work experiences after a cancer diagnosis. Built on the review, we conducted a focus group study to understand nurses' return to work experiences. Our research revealed four key themes that illustrate the return-to-work experience for nurses with cancer:
1. Motivation, incentives, and the need to return to work:
A strong desire to regain normalcy and continue their caregiving roles is expressed by many nurses. For some, the return to work is driven by financial necessity, particularly due to the high costs of cancer treatment.
2. Setbacks hindering the return:
Many lingering treatment side effects, cancer symptoms, along with limited workplace flexibility and job insecurity, posed prominent challenges. Many nurses expressed frustration with navigating employee benefits and inadequate structured support.
3. Navigating new work dynamics:
Nurses acted by adjusting work arrangements, adopting coping mechanisms, and seeking support from family and friends to overcome workplace challenges.
4. Evolving professional role during the return to work:
Adjusting to the dual roles of healthcare providers and recipients of care complicated their return-to-work journey and sometimes caused emotional struggles. Some nurses discovered that their cancer experience empowered them to better empathize with patients and their caregivers and advocate for better care.
Some nurse managers mentioned that they became more aware of staff's needs and more willing to provide adequate support than before.
Potential Solutions to Support Nurses with Cancer
We suggested that to increase return-to-work outcomes for nurses with cancer, interventions should actively target both individual levels and organizational levels. For example, it is critical to help nurses transition back to their roles while managing their health needs by offering multiple modified schedules or several ergonomic adjustments. A more compassionate setting can be promoted by training being provided to managers and colleagues to understand the challenges faced by returning nurses. Structured return-to-work programs, which include peer mentoring or counseling services, can offer costly guidance along with emotional support. Medical leave policies can be structured as clear, accessible pathways for nurses, helping to address systemic barriers to returning to work.
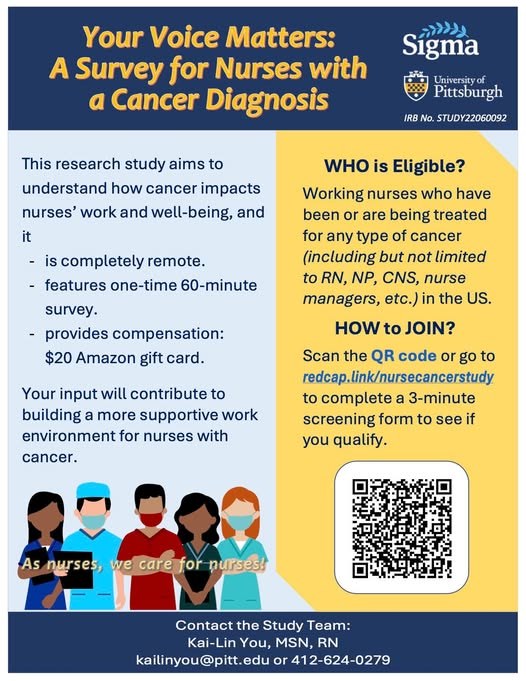
Join our Efforts
We invite nurses who have a personal history of cancer to participate in our research. We are currently working to understand how nurses can be better supported in returning work. Please consider sharing your experiences with our team. Your participation can have positive influence on future support program development. Check out information about the study at our Facebook Page or contact us at [email protected]. Help us spread the work and share this research with colleagues who have experienced cancer.
This is a sponsored article brought to you by allnurses.com in partnership with the advertiser. The views expressed in this article are those of the advertiser and do not necessarily reflect allnurses.com, its parent company, or its staff.