- Community
-
Programs
- Schools
-
Careers
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- NICU Nurse
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Nurse Practitioner
- Best NP Jobs and Salaries
- Family NP (FNP)
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Orthopedic NP
- Emergency NP
- Psychiatric-Mental Health NP (PMHNP)
- APRN
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Resources
- Education

 so pain is a high priority.
so pain is a high priority.
Adelene
11 Posts
I only got to see my patient for 2 1/2 hours before they were discharged home. This patient had bone spurs removed/rotator cuff repaired. Other diagnosis: IDDM, HTN, asthma, and arthritis. The only labs that were abnormal: bedside glucose from the day of surgery: 255 (90 - 110) and a hematocrit of 0.1 higher than normal. Patient was on PCA pump morphine 1mg/ml. Also, three additional PRN pain meds. Was given a total bed bath due to inability to move that side of body. Able to ambulate nursing their arm in a sling. PRN ice packs on affected shoulder. V/S slightly higher than normal. Temp of 100.4 that went down to 98.4 within 2 hours.
Given 1 hour to write down 10 NDs specific to my patient. Number them in order of priority. Pick out 2 physiological and one psychosocial ND - write care plans for each one; must include ND with R/T statements, clinical data supporting ND, interventions with rationales (at least 5 per ND care plan).
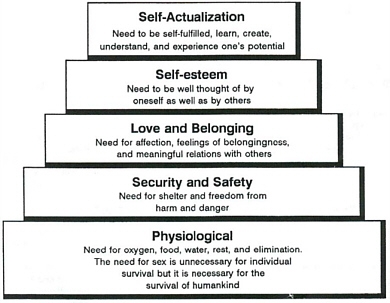
Wanted to use pain as #1, but I was told that instructor said nobody has ever died from pain. Thought about risk for impaired glucose control, but realized that blood glucose of 255 is probably not that unusual for patient (probably NPO, stressed) on the day of surgery. Picked 2 safety and security NDs. Maybe not a good idea?
#1. Impaired skin integrity r/t incisions and tissue trauma from invasive surgical procedure.
Interventions included that diabetics sometimes have more problems with wound healing - may need wound care specialist. Included nutrition with extra protein for healing properties. Exercise for more oxygen capacity for healing. Of course, keep wound clean, dry, and bandaged as ordered. Monitor temp as an indicator of infection.
#2 Impaired physical mobility of shoulder r/t invasive surgical procedure.
Interventions were to give pain med 30 minutes before exercise; go to physical therapy for specific exercises and equipment; allow pt. plenty of time to complete ADLs. Combine activities when possible for less exertion; provide assistance as needed.
Now anxiously awaiting my grade...
Anyone have any ideas?