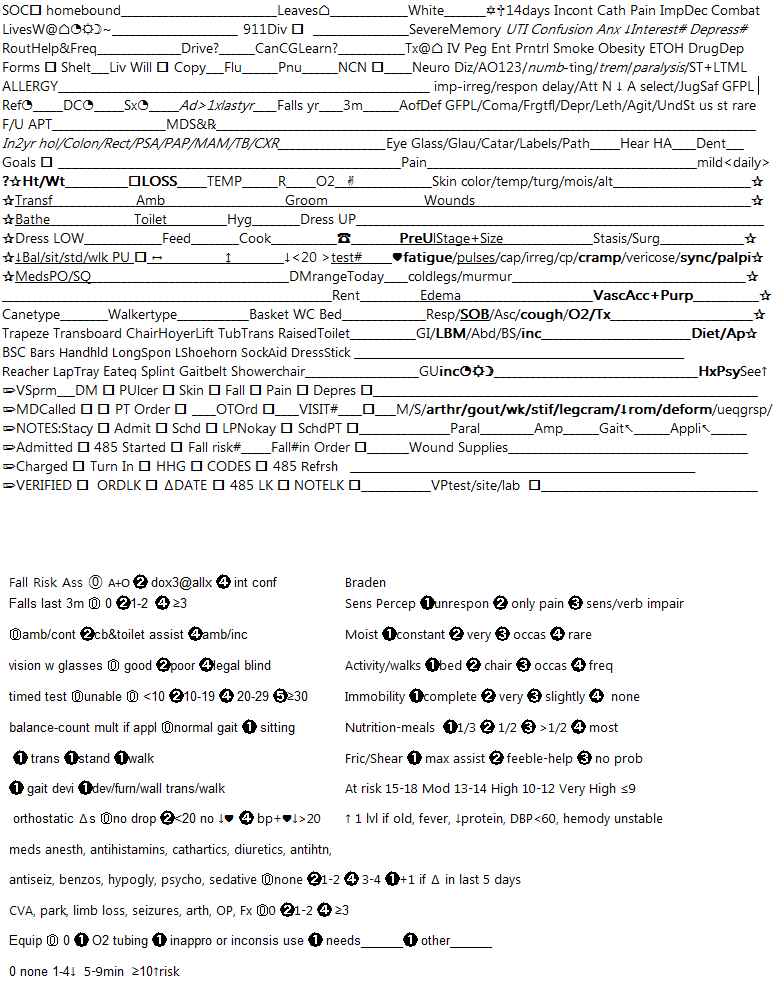
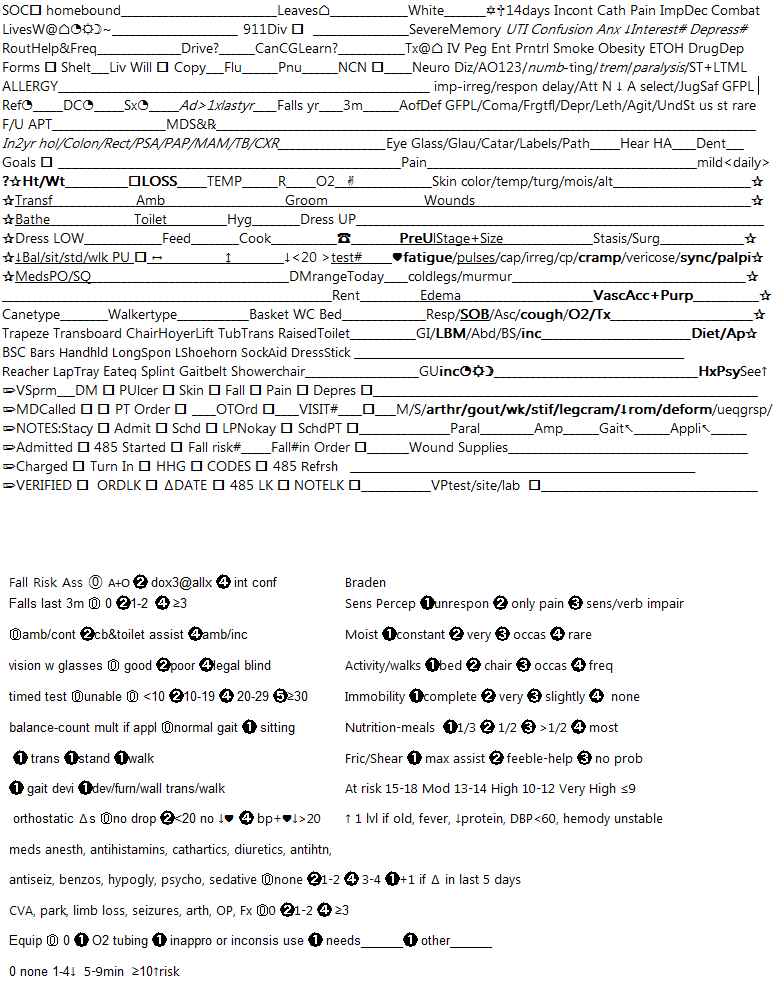
So I'm trying to cover all the bases I'll need to A. have all the assessment data I'll need to fill in the computer forms and B. Have a checklist of sorts to do all the extraneous SOC tasks. Let me explain the shorthand and you tell me what you think or if it is missing anything major. It is meant to be folded in half so that the fall and braden scales are on the back to determine fall risk score and braden score for risk assessment in orders without having to bust open the laptop and then the blank page on the back can be used for notes of whatever kind.
FYI everything with a star next to it requires you to get out of your seat and touch the patient in some way. Everything underlined requires the patient to get up out of his chair. I ask the patient everything I can while they are sitting, and then verify their answers as needed when I have them get up.
Everything with a pencil next to it can be done on the computer outside of the home even though I plan on getting the fall risk assessment # there so I can call the MD right afterward and know whether or not I'm going to be asking for a PT evaluation (we get one if the fall risk is >/10.)
So from the left column top down,
Why is this pt homebound, why do they leave home?
Who do they live with at home; around the clock, during the day only, during night only, occasionally? Who is their emergency contact and is it OK to divulge information to them?
How often to they routinely receive help from a caregiver? Who drives them to appointments? Is caregiver willing and available to learn given care (ie wound care, injections etc)?
Check that forms are signed. Does this patient want to opt in to special needs shelter availability in case of a natural disaster? Does this patient have a living will? Did they give you a copy. When did this patient last have their flu vaccine? Their pneumonia vaccine? check that you document this in the non clinical note for the discharge nurse.
What are this patient's allergies, reactions, and severity of reaction?
What was the referral date for this evaluation? What date was the patient dc'd from the hospital, rehab, etc...if at all? What date was their surgery, if they had one? In the last year, have they been admitted to the hospital more than 1 time? In the last year, how many falls have they had? How many in the last 3 months?
When is their follow up appointment with the referring MD(s)? Who are their other MDs and what pharmacy do they use?
In the last 2 years have they had tests for cholesterol, colon CA, rectal exam, PSA, papsmear, mammogram, tb, and or chest xray?
What is the patient's stated goal(s) for this certification period?
At this point I skip over to the right column and will come back to the left in a bit.
Is the patient Caucasian? (I put white instead of race b/c the majority of my patients are white and it's easier to put a check mark the majority of the time than to write in the race every time) What is their religion (see the little star of david and cross to represent that?) In the last 14 days has the patient had the following: incontinence, urinary cath, pain, impaired decision making, combativeness, severe memory impairment, UTI, confusion, anxiety, decreased interest in doing things, depression (italicized things are used in multiple parts of our computer system and help me to not have to ask the same questions more than once, I have to remember if they say yes to decreased interest and depression to ask them how many days in the last two weeks this has been the case I may put a # sign next to those two to remind me.)
Do they receive IV therapy, peg tube feedings, enteral or parenteral therapy at home? Do they smoke, are they obese, do they have etoh or drug dependency?
Neuro system assessment: do they have dizziness, Are they alert and oriented x 1 x2 or x3, numbness or tingling, tremors, paralysis, is ST or LT memory loss is impaired or irregular, is there a delay in their response time, is their jugement or safety impaired, is their attention span normal decreased absent or selective, (oops looks line I repeated judgement and safety I'll have to fix that) but is it good fair poor or labile, is their awareness of deficit good fair poor or labile, are they in a coma, forgetful, depressed, or lethargic, agitated, do they understand what you are saying usually sometimes or rarely? Anything in neuro those didn't cover? fill in the blank.
Eyes: do they wear glasses, have glaucoma, cataracts, can they read their medication labels with corrective vision in place, if not can they see enough to avoid obstacles in their path? Are they hard of hearing, do they wear hearing aids? Do they wear dentures? I have to remember to ask full or partial and if they have missing teeth if they do not.
Pain assessment, I remember to ask severity on 0-10 scale, what is the best and the worst it gets? how do they describe it, what makes it worse, what makes it better ,what does it keep them from doing, is it acute chronic or recent onset, does the MD know about it, does it radiate, etc... then is it mild enough to not interfere with activity, is it less than daily, daily or constantly?
I ask all I can in interview form below before I touch the patient. interview items are bolded, which I think I will go ahead and do on my form, too. Then I actually go through and physically assess the things that aren't bolded. Remember that underlined things may have to be done either while patient is standing or laying later, for ease of access. So I skip those and come back to them later. Those things are Wounds (it may be easier to do when you have the patient lay down in bed if it is on the leg or stomach for example) Pressure ulcer check (you can't check the sacrum while they are laying down and heels are easier on bed as well) Pulses (pedal pulses and edmay be easier when the patient is laying) SOB (you have to watch the patient breath after movement)
Skin: color, temperature, turgor, moisture, alterations
Wounds: remember to write down size, appearance of peri wound and wound bed, drainage amount and appearance, closure, drains in place, etc... and what you did as far as wound care if it was ordered on referral orders. or if there is a non removable surgical dressing in place.
Do they have a pressure ulcer what stage and size is it? Remember to ask if they have a history of pressure ulcers since anything over a stage III even if healed is assessed and documented forever. Do they have stasis wounds or surgical wounds?
Cardiac: does patient have fatigue, how are their pulses in their extremities, how is their cap refill, leg cramps, vericose veins, syncope, palpitations, are the legs cold to touch, do they have a murmur?
Do they have edema, remember to document location and severity.
Do they have vascular access in place? What is it's purpose and what kind of access is it?
Respiratory: Do they have SOB? (underlined so you can observe) What do you hear on auscultation? Do they have a cough? do they use O2 or respiratory treatments or cpap? remember to document sputum if they have any.
GI: when was their last bowel movement, how does their abdomen feel? How are their bowel sounds, do they have fecal incontinence? What is their diet and how is their appetite? Remember to document ostomy if present and it's size and appearance and part numbers etc...
GU: Do they have incontinence? does timed voiding avoid incontinence? mostly during the day? mostly at night? remember to document any urinary symptoms like burning, urgency etc... also urostomy info as above if present. Blerb to the right is to remind me to document about psychological illess history that is referenced at top of column.
Musculoskeletal: does patient have arthritis, gout, weakness, stiffness, leg cramps, decreased range of motion, deformities, un equal grasps (indicated as a reminder on left column near O2 as a little hand icon), paralysis, amputation, gait (arrow indicating that this is to be assessed and noted on left column), appliances (arrow indicating that this is to be assessed and noted on left column).
I skip Wound supplies and Venipuncture for now and move back to left column. Before you have the patient get up do the starred items that can be done sitting in the chair.
Ask the patient how much they weigh and how tall they are and if they have had a loss recently and how much. Check patients temp and respirations and O2 sat if ordered. Check patient's hand grasps. (the question mark to the left of the star on this row is to remind you that there is a question to ask, ht&wt and loss, the patient here as well as the action of taking those vitals).
Ask the patient how they normally handle the items below from transferring to using the phone. Then ask them how they normally take their PO or SQ meds if applicable. This way you know a little more what to expect when the patient actually gets up.
Now have the patient put his money where his mouth is and GET UP! Tell him to take you to the bathroom where they get up in the morning. Watch him transfer, and ambulate, what device is he using, is there someone there helping him, how much help does he need, how much more help should he be having to be safe? Tell him to pantomime brushing his teeth and hair with his toothbrush and comb. Could he do this if the items in question weren't within reach? Have him get into the shower and pantomime washing his hair, take note of adaptive equipment in place and what he could use that he doesn't have. Have the patient sit on the toilet and show you that he can reach his behind to wipe, does he look steady? have the patient show you where he keeps his clothes and pantomime putting on a shirt and socks. Is he steady? Ask the patient if he feeds himself, who cooks for him? Could he reach his food and microwave safely if he had to? without hands on an assistive device? Without pain putting him at risk for injury? Can he use the phone? Get to the phone?
The next blerb is asking if he had decreased balance while sitting, standing, and or walking, and PU is to remind you to check for pressure ulcer before he sits back down.
Now is where I have them take me to where they sleep and lay down in their bed. the horizontal arrow is indicating laying BP and heartrate. It's at this time that I Do the underlined things on the right column. Wound assessment and wound care, writing down wound supplies, checking sacrum and heels if they are too unsteady to check while standing, pedal pulses, leg edema. Then I do standing BP and heart rate, indicated by the vertical arrow. Did their pressure drop 20 points? Then I have them sit back on the bed and do the timed up and go test. Get up, walk 10 feet, come back and sit down. How many seconds did this take? scoring on back.
Now I have them take me to their meds and walk through them with me. Read me the med names tell me what they are for and when you take them. I do the med rec at the same time. I ask if they are diabetic what is their normal range of FSBS and what was it today, if they check it? Do they draw up and inject it themselves?
I ask them if they have the eqipment listed below, if any of it is rented, and I verify what they say with what I saw when we took our walk.
At this time I take blood if ordered and write it down at the bottom of the right column.
Venipuncture what test was drawn, from what site, what lab did you drop it off to? check box that you documented it.
I grab my forms and cheat sheet, thank them for their patience, tell them I will be calling their doctor for orders and what orders I will be asking for, and tell them someone will be calling to set up their next visit and when I anticipate that to be, although nothing is written in stone.
Then I leave and go somewhere comfortable (probably my car, LOL, although starbucks would be nice, it's always crowded.) And do some of the pencil things. Let me go through and explain what they all are.
VSprm: are there any vital signs or other parameters I think the doctor should put on the patient? BP? Weight? FSBS? Does the patient have the following? DM, pressure ulcer, high skin risk according to braden score, fall risk according to scale, pain, depression hx or indicators
Call the MD first check box is you put a call out, second is they called you back. Did you get a PT eval order? or was there one already? the line next to that is how many visits the PT thinks they need after they do their eval so you can put it on the oasis along with OTorder which means either OT visit number or "other" such as social worker etc... Total number of other discipline visit estimate according to the orders they put in goes in Visit # so you can put it on the oasis.
Put in notes to your coder (ours is stacy), a general admission note for the case manager, a note to scheduling to generate visits for orders when in, and a blerb on whether or not this patient is appropriate for an LPN to see in that note, and a note for PT eval visit generation for schedulers.
Mark the patient as admitted, start the 485 once you get your orders, make sure to put the fall risk # in the order to justify PT eval or absence of one due to risk, charge the patient for supplies used or left in home, turn in signed paperwork, HHG is a form we get emailed to us to reconcile irregularities in charting and evaluate if we would like to change them. Enter codes when they come in from coding company and enter severities, refresh the 485 to include codes, get the OK from your supervisor to lock down charting, and lock down order, change the date on the bottom of 485 to reflect SOC date, lock 485 and lock visit note.
Phew, it looks like so much less when written in short hand! Any suggestions for improvement of my cheat sheet or process?
Thanks!


mrod15
5 Posts
If you want to use these cheat sheets then I would add "laterality" to some of these. For example wounds and such. Laterality is HUGE for ICD-10 coding/485.